In this episode, host Nicole Weathers is joined by Dr. Kirsten Hanrahan and Dr. Laura Cullen from University of Iowa Health Care to explore how evidence-based practice (EBP) can empower new graduate nurses rather than intimidate them. Together, they unpack the Iowa Model, clarify the differences between EBP, quality improvement, research, and innovation, and share practical strategies for supporting new nurses through their professional experience projects. Whether you're a nurse leader or a recent grad, this episode offers valuable insights to make EBP approachable and impactful.
GUESTS:
Kirsten Hanrahan, DNP, ARNP, CPNP-PC, FAAN
Director, Nursing Research & Evidence-Based Practice
University of Iowa Health Care
Evidence-Based Practice Resources | University of Iowa Health Care
Kirsten Hanrahan, DNP, ARNP, CPNP-PC, FAAN, is the Director of Nursing Research and Evidence-Based Practice for the University of Iowa Health Care. Dr. Hanrahan is well-versed in EBP, clinical research, and innovation. She has numerous publications, national and international presentations, and has been named one of Iowa’s 100 Great Nurses, a 2019 Fellow of the American Academy of Nursing, and a 2020-2021 Mayday Pain & Society Fellow.
Laura Cullen, DNP, RN, FAAN
EBP Scientist
University of Iowa Health Care
Laura Cullen, DNP, RN, FAAN, leads Evidence-Based Practice at University of Iowa Health Care. Laura is internationally recognized for her expertise in EBP and implementation. Among her many accomplishments, she is most proud of the many clinicians she has mentored and of staying application-oriented. Laura’s work has led to innovation in practice, improved patient safety, reduced nosocomial events, improved patient, family, and staff satisfaction, reduced hospital LOS and costs, and transformed many organizations’ EBP infrastructure. She has over 100 publications and presents nationally and internationally. Laura has a regular EBP column in the Journal of PeriAnesthesia Nursing, is on the editorial board of the American Journal of Nursing, and has been on the grant review panel for the DAISY Foundation. She has received multiple awards, and her work has supported numerous awards for the nursing department.
Articles or Publications: Cullen, L., Hanrahan, K., Edmonds, S., Reisinger, H., Wagner, M. (2022). Iowa Implementation for Sustainability Framework. Implementation Science,17:1. https://doi.org/10.1186/s13012-021-01157-5
Cullen, L., Hanrahan, K., Farrington, M., Tucker, S., & Edmonds, S. (Eds.). (2023). Evidence-based practice in action: Comprehensive strategies, tools, and tips from the University of Iowa Hospitals & Clinics (2nd ed.).
ORDER BOOK
Hosking, J., Knox, K., Forman, J., Montgomery, L., Valde, J., Cullen, L. (2016). Evidence into Practice: Leading New Graduate Nurses to Evidence-Based Practice Through a Nurse Residency Program. Journal of PeriAnesthesia Nursing, 31(3), 260-265.
Iowa Model Collaborative (2017). Iowa Model of Evidence-Based Practice: Revisions and Validation. Worldviews on Evidence-Based Nursing, 14(3), 175-182. doi: 10.1111/wvn.12223.
Supporting nurses is our priority. Visit https://nursing.uiowa.edu/ionrp to explore our resources for new graduate nurses and beyond.
 1 時間 10 分
1 時間 10 分 1 時間 8 分
1 時間 8 分 51 分
51 分 57 分
57 分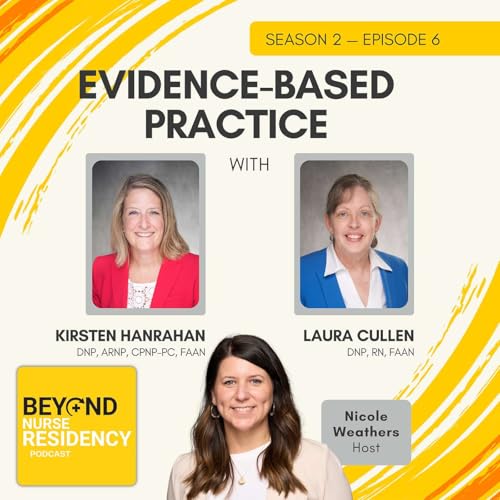 2025/06/011 時間 1 分
2025/06/011 時間 1 分 54 分
54 分 2025/04/0148 分
2025/04/0148 分 53 分
53 分
